Mapping Neuroethics: An Expanded VisionThe 2019 Annual Meeting of the International Neuroethics Society (INS) gathered a diverse group of scholars, scientists, clinicians, and professionals dedicated to the responsible use of advances in brain science. Attendees participated in intellectually stimulating and dynamic sessions that explored neuroethics in a global context.
Sponsors     Overviews
Previews
 Meeting Photos Many thanks to Gillian Hue for capturing key moments from the annual meeting. Several great photos are available at the bottom of this page. Other photos from the meeting are available upon request for personal or professional use. Contact staff by email ([email protected]) with your requests. Please be sure to credit Gillian Hue when sharing photos online.
Plenary Speakers
 FRED KAVLI DISTINGUISHED NEUROETHICS LECTUREMartha J. FarahCenter for Neuroscience & Society
 OPENING PLENARY SPEAKERMatthew L. BaumHarvard Medical School
Sessions
Solving Dilemmas in Global Neuroethics Presentations and a follow-up world cafe discussion with the full audience examined several themes addressed in the perspective article, 'Neuroethics Questions to Guide Ethical Research in the International Brain Initiatives' (Neuron, 2018). The goal of this session was to promote a productive dialogue on diverse ethical approaches to contemporary issues in global neuroethics.
Ethics and the Imprisoned Brain As researchers begin to investigate techniques for altering inmates' brains to rid prisons of what Anthony Burgess called ‘the ultra-violence,’ the ongoing neuroethics discourse about biological approaches to criminal justice takes on renewed urgency. Speakers addressed the promise and peril of neuro-interventions for incarcerated persons, whether in research and development or implementation and oversight.
Incapable Patients and Psychiatric Neurosurgery: What do Law and Ethics Have to Say?
Preclinical Interventions in Psychiatric and Neurological Disorders As we get better at using genetic, metabolic or behavioral biomarkers to predict future susceptibility for neurological and psychiatric syndromes, the problem of medical management of people in such preclinical states becomes more trenchant. Testing preventive drugs, informing patients or parents of risks, managing false positives, and treating patients with little discernible illness raise significant ethical questions that were discussed with a panel of experts.
Disorders of Consciousness: Concepts, Culture and Prognosis
SUMMARIESMartha Farah honored for her service to the field of neuroethicsMartha Farah, the Walter H. Annenberg Professor in Natural Sciences and professor of psychology at the University of Pennsylvania, is the 2019 winner of the Steven E. Hyman Award for Distinguished Service to the Field of Neuroethics. Professor Farah has degrees in metallurgy and philosophy from Massachusetts Institute of Technology and a PhD in psychology from Harvard University. Now she is a cognitive neuroscientist and her research focusses on socioeconomic status (SES) and brain development. SES is linked to the way we think and solve problems and to our well-being and mental health. She is a founding director of the Center for Neuroscience and Society at the University of Pennsylvania. Professor Farah was also one of the founders of the International Neuroethics Society. 
Steve Hyman, awardee Martha Farah, Hank Greely, Nita Farahany and Judy Illes. The INS established the Steven E. Hyman award in 2016 to recognize people who have helped develop the field of neuroethics and who have contributed to the INS. The INS President, Immediate Past President, and President-Elect select the recipient. Professor Hank Greely, now the INS Immediate Past-President, said, "Martha has been part of the INS since it was established in 2006. She has played a crucial role within the INS, and in neuroethics more generally outside the INS." Presenting the award at the INS annual meeting in Chicago on Friday, October 18, Professor Steve Hyman, for whom the prize is named, said, "We are delighted to present this award to Martha Farah, a world-leading cognitive neuroscientist. Her pioneering work on the link between poverty and children’s brain development is neglected by the neuroscience community, and yet her research is what neuroethics should be about." Receiving the award, Professor Farah said, "I feel very honored by this award, named for one of my neuroscience and neuroethics heroes. I am also very grateful to the INS leadership, who have done so much to advance the understanding of ethics in neuroscience. Their approval means a lot to me!" Should we trust technology to provide mental health care?The public program, organized by the International Neuroethics Society in conjunction with Northwestern University, examined the potential challenges and opportunities associated with digital mental health care. Based upon our increased reliance on technology, can we trust technology to supplement, or eventually substitute, human health care providers? 
Public program meeting room at the Daniel Hale Williams Auditorium at Northwestern University Mental illness accounts for approximately one-third of global adult disability (Lake, 2017). The number of individuals diagnosed with mental health disorders continues to increase worldwide, with a substantial proportion of individuals failing to receive any treatment. In the United States, approximately 1 in 4 adults suffer from a diagnosable mental health disorder, and 44.7 million U.S. adults were diagnosed with a mental health disorder in the last year, with only 43 percent receiving mental health treatment. Moreover, approximately 10.4 million U.S. adults were diagnosed with severe mental health disorders, such as major depressive disorder, anxiety disorders, bipolar disorder, schizophrenia, and substance use disorders, but only 6.7 million received treatment. Worldwide, more than 70 percent of individuals with mental illness do not receive mental health treatment (Henderson et.al, 2013). Mental health services are often unavailable or underutilized in developed countries. There are several barriers to receiving mental health services, including lack of knowledge to identify characteristics of mental illnesses, stigmatization of those with mental illness, and the expectation of discrimination against those diagnosed with mental illness. Digital Mental Health Technology: The Potential to Improve Quality and Access of Mental Care Nicole Martinez-Martin highlighted the great potential of digital technology to improve the quality and overall use of mental health care. There has been significant investment in mental health startups, with the mental health sector receiving a record-breaking $602 million in funding last year. Approximately 77 percent of mental health startups companies were focused on mobile applications. These mobile applications are not only intended for clinical use, but for consumer use as well. However, actual consumer use can trail behind health technology innovation. Although many people may use the internet and mobile health applications for wellness and information gathering, very few use it to interact with their health care provider or insurance company, a survey by Kaiser Family Foundation found. Some ethical challenges associated with digital mental health therapy include safety/accuracy, privacy, accountability, bias/fairness, informed consent, transparency, incidental findings, and the therapeutic alliance. She also emphasized the importance of trust in health care and technology. The concept of trust, often invoked but not necessarily explored, is multi-dimensional and heavily dependent on context. Trust invokes relational obligations and vulnerability, in which an individual must place their trust in another individual or entity to further their interests. These relational obligations are heavily observed in the healthcare context, as trust can manifest in the patient–physician relationship and within interactions with healthcare institutions. In discussing digital mental health technology, trust is heavily associated with the trustworthiness of technology companies. In terms of mental health therapy, trust and trustworthiness are inextricably linked to ethical care. Some major dimensions of trustworthiness in mental health therapy include disclosure, confidentiality, dignity, continuity of care, safety avoidance, treatment effectiveness, and avoidance of stigma and coercion. These perceptions of mutual trust are crucial to the therapeutic relationship. These applications can be used as a platform for connecting with clinicians, licensed therapists, life coaches, or peers. Some forms of mobile applications include wellness apps (e.g., meditation, information for self-guided care), mood-tracking (self-monitored or monitoring by a physician), medication information/tracking, or conversational agents. It matters whether mobile applications are used within clinical or consumer domains. Whereas clinical domains require information confidentiality under HIPPA, consumer domains have been described as the ‘wild west’ with regard to data protections. Different ethical obligations will be imposed depending on the given context in which mobile applications are used. Individuals who use these mobile applications may not be aware of the behavioral inferences that can be drawn from information and its potential repercussions. Given the large demand for data, personal health information can be generated outside of HIPAA protections, exposing consumers to privacy breaches. Due to the complex nature of mental and psychological illnesses, interventions will require multifaceted approaches. Digital mental health technology has the potential to deliver mental health care on an unprecedented scale, supplementing care to provide more comprehensive mental health interventions. Digital mental health technology could potentially resolve the challenges associated with traditional mental health care, bridging any gaps in mental health treatment. She recommended that digital mental health therapy be deployed in an accountable, fair, and transparent manner and that oversight and protections must be considered for both patient and consumers alike. Being Human: A Challenge for Mental Health Digital Interventions Approximately 1 in 3 individuals worldwide have a mental health illness. Those living in developed countries often receive little to no treatment. Dr. Singh began by explaining her current empirical study focusing on early intervention in psychosis (EIP). The early intervention psychosis program is suited towards those who experiencing symptoms of psychosis for the first time and younger individuals with at-risk mental states. The early intervention paradigm focuses on the early identification and treatment of younger pre-symptomatic individuals who are at high risk of developing their first psychotic episode. The study employed a virtue ethics framework, finding that: negative moral self-understandings have significant consequences for the potential for recovery; EIP services are linked with ‘moral mastery’ and more positive moral self-understandings; and talking and listening is fundamental to good practice and can lead to more positive moral self-understandings. This third finding led to another important question: what ethical challenges exist in replacing mental health therapists for digital applications? The empirical data consistently indicates that the therapeutic relationship itself is strongly associated with successful patient outcomes. These psychotherapeutic benefits emerge from storytelling, which is a crucial component of the intervention process. The ability to express one’s personal story is fundamental to self-understanding and self-reflection. Through storytelling, many people gain vital insight into their lives that can lead to direct behavioral change and thus vast improvement in their quality of life. Her presentation later examined the future role, or lack thereof, of human specialists in digital mental health interventions. Since the therapeutic relationship is grounded upon human interaction, what would be the implications for digital mental health interventions, where there is no active human component? Dr. Singh describes the therapeutic relationship is a uniquely human encounter. Are human beings required for digital mental health interventions? Could artificial intelligence (AI) stand in for humans in the digital mental health clinical encounter? If so, how ‘human’ should the AI be? Human interaction is not required for every mental health intervention. AI could serve to be more useful than humans in mental health intervention in terms of efficiency, errors, and bias. In contrast, human interaction could be more preferable for treatment of mental disorders that cause feelings of inhumanness, such as psychosis. Is it possible to build ‘good-enough’ AI interventions? If so, how would the ‘good-enough’ AI interventions be distributed? Digital Mental Health Dr. Mohr’s presentation focused on the application of personal sensing — or digital phenotyping, which involves harnessing digital fingerprints from personal digital devices to understand behavior — to digital mental health interventions. Given their widespread ownership and diverse usage, smartphones can be used as a lens to predict mental status and understand behaviors related to mental health. However, a major issue with mobile health applications, which are largely feedback devices, is low data input from users. He advocates for the development of simple mobile applications that nudge behavior in positive directions, a marked departure from the concept of creating specific mobile applications for each mental health disorder. Several randomized controlled trials suggest that the outcomes received through digital mental health interventions mirror that received through traditional interventions, such as pharmacotherapy or psychotherapy. Some challenges associated with digital health interventions include low patient acceptance and lack of integration into care systems. The design of current digital mental health intervention is heavily based on psychotherapy. The translation of psychotherapy into a digital platform, he argues, is fundamentally wrong since it undermines the therapeutic alliance. There are several inherent weaknesses to digital mental health applications. Data can be extremely revealing, and consumers often cannot effectively manage their privacy. Many of these applications do not have robust privacy policies in place to protect users. Additionally, most mental health applications do not have review processes, and many are not evidence-based or based on sound psychological principles. He asserts that society is on the cusp of a technological revolution with digital mental health interventions, due to its potential cost effectiveness and ability to increase access to mental health treatment. For this to occur, however, there needs to be marked paradigm shift in mental health conceptualizations. He recommends that app developers and health systems collaborate with patients and experts from other disciplines to examine how personal sensing can be safely integrated into clinical practice. Summary written by Kimberley Glover Incapable Patients and Psychiatric Neurosurgery: What do Law and Ethics Have to Say?Many laws define psychosurgery to include deep brain stimulation (DBS) for psychiatric indications, a field under intensive exploration and expansion. This session considered the history, present and future, of the regulation of invasive psychiatric neuromodulation such as DBS, with particular attention to the questions of whether there is a need for specific law, and what its optimal contents should be.
Professor Jennifer Chandler introduced the panel and started the conversation by describing how her interests for psychiatric neurosurgery started when discovering the varying procedures and legalities for obtaining informed consent for psychosurgery around Canada, Australia and the United States. She asked how the cultural understandings of psychiatric neurosurgery might have originally prompted these laws and if such laws are protecting patients or hindering their access to these vital treatments. Dr. Laura Cabrera started the panel by stating her goal was originally in line with Professor Chandler's question of understanding whether psychiatric neurosurgery ought to be regulated. Understandably this question has intrinsic importance given the risk of personality modifications with psychosurgery. She cited a 1949 article that articulated how the medical community should regulate themselves on the use of these procedures, given their thorough knowledge of it. However, this stance gradually changed through the later parts of the 20th century following abuse of psychosurgery and other medical research studies. This prompted intervention by the courts to mandate complete disclosure of the pros and cons of psychosurgery to the patients and around limitations on who could give consent following such disclosures (i.e. those without reasonable levels of autonomy). Specifically, regarding the second concern, the courts pressed that those with psychiatric disorders were likely incompetent to make an informed choice or independent autonomous decision due to their current residence in a mental healthcare facility and the possible effects of coercion. Dr. Cabrera described that Oregon was the first to set actual standards of consent for psychosurgery.She also questioned the notion of defining ‘procedure(s)' within the law, as only six states with legal regulations on psychosurgery defined this term and that even these definitions were too ambiguous and includednoninvasive neural stimulations within their definitions. She stressed that this definition may improve with narrowing to invasive practices and by following prior recommendations for institutional review board or regularity oversight for these procedures with high standards for informed consent. Dr. Cabrera concluded her talk by highlighting the lack of enforcement for these procedures when considered or performed outside of the established guidelines. She stressed the need to develop more rigorous ethical protocols to guide the use of such therapies outside established patient populations in a way that does not overly limit their potential benefit to other patients. Lauren Sankary, JD, focused the conversation of psychiatric neurosurgery to those procedures conducted in the research setting for deep brain stimulation (DBS). She described her own research surrounding the end of trial research procedures with these neurostimulation devices. She drew questions about the implicit ambiguity and ethical weight given to DBS for a psychiatric disorder over more classic and neutral disorders like Parkinson's disease. She then posited her main ethical concerns of therapeutic misconception with trial enrollment, continued care for patients following completion of research trials (i.e. still utilizing the implanted neurostimulation device), and the possibility of creating a vulnerable patient population following neurostimulation due to compromised neurophysiological networks necessary for autonomy. To address the first concern, she recommended future empirical neuroethical research to quantify the characteristics of vulnerability to better discover what aspects might be best improved through regulation. Regarding the second ethical concern, she had wanted to understand the ethical obligations of researchers towards continued care. She found, through her prior research, the need for researchers to maintain a level of autonomy, free of coercion, to participants by allowing and providing access to neurostimulation device removal. This was contextualized by the qualitative findings about how patient's felt overwhelmed by the shear amount of information provided to understand at the onset of the trials. Also realized through this research was the uncertainly when researcher responsibilities end following the completion of the trial and how the difficulty of institutional review boards to enforce researcher responsibility compounds the issue. She provided patient feedback containing concerns about who would support their continued use of the devices and a feeling of being disconnected from the researchers they had established a professional relationship with through the trial. She concluded the presentation by highlighting the ambiguity within DBS end-of-trial procedures on matters of autonomy and justice, but didn't stress the need for further regulation. 
Lauren Sankary, Laura Cabrera, Jennifer Chandler and Eran Klein Wrapping up the panel was Dr. Eran Klein. He introduced his presentation and after a brief introduction of DBS he asked about the future concerns of psychiatric neurosurgery. He drew from the development of the ethical questions for DBS over the past century and specifically addressed an article articulating the seven common trends of these questions. He blended these trends with qualitative data from patient experiences he had collected with the Neuroethics Thrust at the Center for Neurotechnology. The first topic of ethical oversight stressed continued review of DBS research procedures, namely Institutional review boards. However, Dr. Klein reported a patient feeling that the Institutional review board was present for protection of the intuition rather than the individual participants. The second topic surrounded experience and interdisciplinary teams, and relates largely to clinical effectiveness; however, Dr. Klein posited the concerns about resource scarcity with such important treatments being focused in condensed locations. The third and fourth ethical concerns related to patient selection, which was defined as the need for strict enrollment criteria with high-risk trials, and also the overall obligations of researchers to provide participants with continued care. Similar to how Sankary stressed in the in her talk, a patient interviewed by Dr. Klein described the researcher's ethical obligations to him and his health because they were about to put this device in his head. The fifth ethical concern involved conditions of informed consent to determine topics like decisional capacity or desperation. However, almost paradoxically, Dr. Klein highlighted how with the advanced levels of depression required for enrollment in some DBS trials, that the topic of desperation was brought up often since most patient's already saw this as their ‘last hope' of a therapeutic improvement. The two final topics included social responsibility, such as using research practically and therapeutically, and scientific practices, or the need for high standards of academic rigor. Dr. Klein shifted his presentation towards future developments with neurotechnology including patient control of medical devices where, for example, Bluetooth could allow more remote access to neural or medical data by providers. These could one day include medical information that is downloadable and able to be sent to providers for convenience, while at the same time increasing the ethical concerns of misdiagnosis and data security. A second future development he discussed regarded increasing levels of customizability of neural devices that would then allow patients to make their own neural adjustments. Importantly, Dr. Klein noted that in such a scenario the acceptable range of neurostimulation would still need to be determined. He also noted how some patients he interviewed were skeptical of such control out of concern for developing addiction-like behaviors. Finally, he noted future advances in DBS may continue to utilize a closed-loop DBS design where the devices function is almost entirely independent of the patient and clinician. In closing, he described that with closed-loop DBS devices the patient–clinician relationship may become unnecessary through the duration of treatment. He described this situation as: "why have an apple a day [to keep the doctor away} when you could have machine learning ?" Lastly, he articulated the interesting neuroethical questions about closed-loop DBS devices used tangentially, with the family's feedback, and how that patient's identity is perceived both by themselves and their loved ones. As these topics mature, and technological advances become crystalized, more subtle ethical questions may emerge. Summary written by Ian Stevens Works cited:
Disorders of Consciousness: Concepts, Culture and PrognosisThis session explored the importance of concepts when addressing disorders of consciousness. Speakers discussed the cultural dimensions and ethical implications of selecting concepts, how concepts can impact practice protocol and medical decision-making, and the potential consequences of categorizing patients. Speakers included:
Dr. Hannah Maslen introduced the panel by first questioning the underlying importance of having different concepts and terms to describe a patient's level of consciousness within medicine. She answered her rhetorical question by pointing to its importance on the diagnostic spectrum to accurately describe a patient's level of awareness but also on a prognostic level to generally predict their chance of recovery. However, her answer was ambiguous, as she questioned if contemporary concepts of consciousness accurately performed these tasks or if modification was needed to provide further clarity. She also emphasized the capacity of these concepts to account for unknown risk, given the general difficulty in diagnosing a patient's level of awareness given its subjective nature. Dr. Joseph J. Fins began his presentation by emphasizing the historical context of disorders of consciousness and the development of today's American Academy of Neurology (AAN) practical guidelines from the prior forty years of academic rigor. Such developments occurred through interdisciplinary discussions between the AAN and American College of Rehabilitative Medicine, among others, to call for improved diagnostic imaging and management of co-morbidity complications in these patient's recovery. Dr. Fins emphasized the shift in diagnostic nomenclature from describing patients in a permanent vegetative state to those in a persistent or chronic vegetative state and the significant difference in prognostic implications this had. Importantly, he noted how permanent nosology implied a prognosis while persistent indicated a diagnosis. Dr. Fins notes the hesitancy of previous scholars to grant higher levels of awareness that was clinically undeterminable. However, the understanding of these terms was only compounded by contemporary developments in neuroimaging where the patients may present minimal awareness, but their neural activity is paradoxically active. This, what was later termed cognitive motor dissociation, complicated the diagnostic picture by expanding the assessment criteria beyond simply behavioral assessments. Unfortunately, he cites the prominence of inaccurate diagnoses when incorporating neuroimaging techniques and stresses the vulnerability of this patient population who might be aware but otherwise unable to communicate such facts. He synonymously noted that the simple presence of consciousness with sentience out of concern for maleficent actions. Thus, he concluded with positing evaluative recommendations of beneficence in the face of ambiguous diagnostic data to best respect the patient's possible level of sentience. 
Joseph J. Fins, Laura Specker Sullivan and L. Syd M Johnson Dr. Laura Specker Sullivan started her presentation describing the complexity of consciousness and how it includes philosophical topics such as self-awareness, alertness, and perceptiveness. When examining biological beings for consciousness, she continued, the prominent dimensions of assessment include wakefulness and awareness. Wakefulness is synonymous with arousal where awareness is understood when someone has an object of their perception. This is best seen in vegetative patient's where they have levels of wakefulness but are absent awareness. She stressed that contemporary concern about patients being in a minimally conscious state stems from the fact that culturally we place ethical importance on awareness, however minimal that awareness may be. Assessing degrees of awareness, as discussed in Dr. Fin's lecture, has only become more complicated and nuanced with the use of neuroimaging techniques. Dr. Specker Sullivan further examined the philosophy of mind contrasting sentience, the ability to experience good or bad states, to sapience, which is a human's rational mind. She also contrasted transitive consciousness, or awareness of an object, to intransitive consciousness, which is understood as pure experience, much like meditation. She, then, questioned the implicit ethical value our culture gives to consciousness that is grounded in its internal value and sometimes its instrumental value for pleasurable experiences. Each of these justifications have their own ethical recommendations. She tied these topics together by describing that when patients simply retain a level of wakefulness there may be an ethical imperative to protect them due to the intrinsic value of consciousnesses. She describes that diagnostically confirming this is still a clinical challenge with it hard to prove that some level of transitive conscious isn't present. Thus, given this varying clinical uncertainty, she recommended the focus should be on examining if patients are sentient beyond the complicated question of their state of consciousness, which is in line with classical bioethical notions of beneficence. Dr. Syd Johnson began her presentation discussing the historical pace of disorders of consciousness moving from the 1970s to a more staggering pace in the past two decades with the identification of Unresponsive Wakefulness Syndrome and cognitive motor dissociation. She questioned if current clinically diagnostic categories are now ethically adequate to encompass the vast variety of conscious states and their moral nuances accumulating in the medical community. She stated that we are currently in an age of uncertainty regarding medical understandings of consciousness due to the increased implementation of diagnostic criteria with neuroimaging. She contends that the ethical notions have not kept pace with this scientific growth and cites historical uses of ethical risks in the philosophy of science being used to increase the level of skepticism towards a notion of truth (due to the levels of deleterious consequences that could result). This leaded her to advocate that with epistemic uncertainty, scholars ought to be more careful in their bioethical or neuroethical risk taking since consciousness matters in respect to many factors, including personhood. She gave an example of such risk with the notion of the vegetative state being culturally sensitive due to its social understanding as "more dead than dead." Thus, she recommended, as the diagnoses of the disorders of consciousness continue to progress, that they include more accurate assessments of risks in their nomenclature. Summary written by Ian Stevens References:
PhotosMany thanks to Gillian Hue for capturing key moments from the annual meeting. Other photos from the meeting are available upon request for personal or professional use. Contact staff by email ([email protected]) with your requests. Please be sure to credit Gillian Hue when sharing photos online. 
Nita Farahany and Matthew Baum after his lecture titled 'The Neuroethics of Biomarkers' 
Emily Largent speaking at the Preclinical Interventions in Psychiatric and Neurological Disorders session 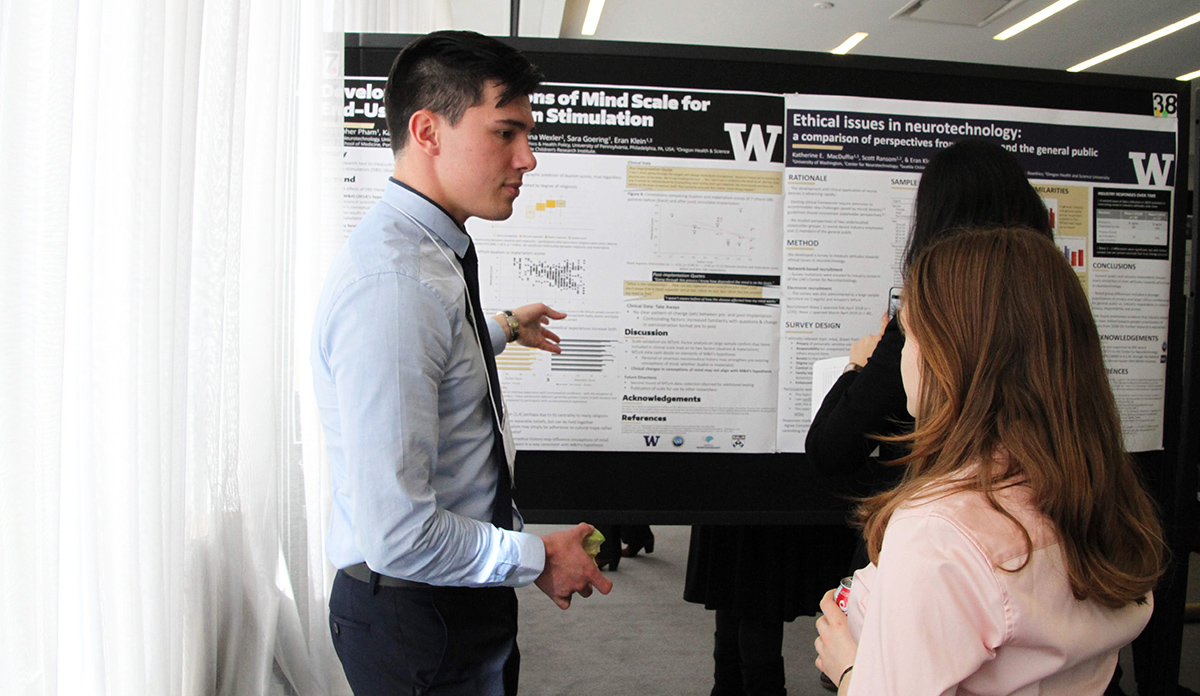
Christopher Pham presenting his poster to Deena Kopyto 
Shelly Benjaminy and Ian Stevens at the poster presentation session 
Attendees participating in the Global Neuroethics roundtable discussion 
Michael Patterson presenting essay contest winners Khayla Black, Sunidhi Ramesh and Prithvi Nathan, with Hank Greely 
Public program speakers Nicole Martinez-Martin, Ilina Singh and David C Mohr |
